Understanding Your Baby’s Fetal Position for Birth
Clinically reviewed by Cindy Richardson, CMPE.
What Is Fetal Positioning?
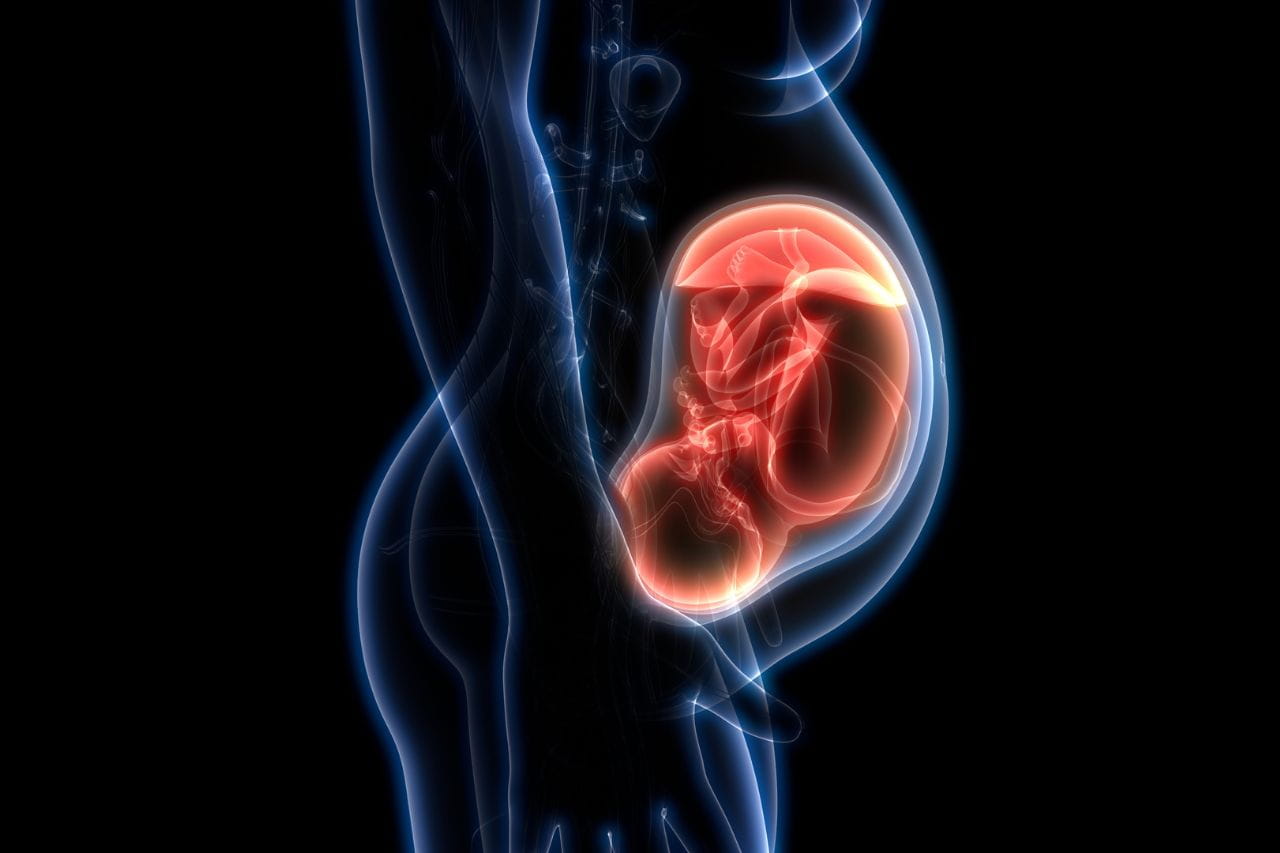
Fetal positioning is the orientation of the baby in the womb. Throughout pregnancy, fetal positioning will often shift. As it gets closer to delivery, the positioning of the baby becomes much more important. Where the baby is positioned in the womb will indicate whether a vaginal birth is safe, or if a C-section is needed.
Why Fetal Position Matters for Birth
Until the last month of pregnancy, a fetus’ position is relatively unimportant. A baby typically has plenty of room to move around in the womb for the first 7-8 months.
In the last month, they’re big enough that movement is more difficult. And the baby’s position in the womb as a pregnancy approaches full term is important since their orientation can make delivery easier or more difficult.
Depending on the fetal position during delivery, your doctor will determine whether a vaginal birth is safe, or if a C-section is needed. The most optimal fetal position for birth is occiput or cephalic anterior. This means the baby’s head is down and facing the mother’s spine. The baby’s chin will be tucked and the head will be facing left or right. If the baby is breech, or if the baby is lying sideways across the uterus on its back (transverse lie), a C-section will be recommended for a safe delivery. Any misalignment of the baby in the uterus at the time of delivery may pose a risk to the mother and baby.
Primary Positions for Babies in the Womb During Delivery
In the weeks leading up to their birth, babies typically assume one of four positions.
Occiput or Cephalic Anterior
This is the best position for a baby to be in before delivery. Their head is down, and their occiput (the back of their head) is toward the front (anterior) of your body. Some people describe it as having their head down and facing your back. This position can be subdivided into left occiput anterior and right occiput anterior, depending on which side of the womb the baby is on.
When the baby’s head is down and facing the mother’s spine, and the chin, arms, and legs are tucked, it poses the least amount of risk in delivery. The left occiput anterior (LOA) means that the baby is in this position with its head facing left, and the right occiput anterior (ROA) means the baby’s head will be facing right. Additionally, the LOA is the most preferred and optimal positioning, as it aligns best with the mother’s anatomy. However, both of these positionings are conducive for a safe and smooth labor and delivery process.
Occiput or Cephalic Posterior
This position is when the baby is head down and facing the front. In many cases, they’ll rotate to face the back on their own before delivery. If they don’t, the occiput posterior position increases the likelihood of prolonged labor and significant back pain.
In some cases, an epidural might be needed to reduce the pain.
In a left occiput posterior (LOP), the baby’s head will be down and facing the mother’s stomach. The baby’s head will also be facing left. In a right occiput posterior (ROP), the baby’s head will be facing right. Both the right and left occiput posteriors are often referred to as “sunny side up.”
A vaginal birth may still be safe with this positioning. However, in this positioning, the baby has a harder time tucking its chin to move down the birth canal. Often, in this position, the labor process takes much longer, and sometimes a C-section may be recommended.
Your doctor may recommend certain postures or exercises before the labor and delivery process to try and get the baby to move into a more optimal position. Sometimes gentle stimulation with sound (music, talking, etc.), light, or temperature changes may also cause the baby to shift positions.
Breech
The breech position is when the baby’s head is up. There are three types of breech positions:
- Complete breech. The baby’s buttocks are pointed toward the birth canal with its legs bent and feet near the buttocks.
- Frank breech. The baby’s buttocks are down, and their feet are up near their chest.
- Footling breech. One or both feet are pointed downward toward the birth canal.
Most breech babies are born without complications, but problems can occur since the head is the last part to emerge. This increases the risk of trauma and congenital disabilities. The breech position also increases the risk of a loop forming in the umbilical cord and harming the baby.
Your doctor may attempt to change your breech baby’s position in the final weeks of pregnancy. They do this using a procedure called external cephalic version (ECV), in which they apply external pressure to your abdomen. It’s successful roughly half of the time.
The procedure can be uncomfortable for you but isn’t dangerous for you or your baby. Still, your care team monitors the baby’s heartbeat and will stop the process if there are any signs of stress.
If ECV isn’t successful, your doctor may recommend a cesarean delivery (or C-section) to protect your baby. That’s especially true if they’re in the footling breech position. The risk in that orientation is that the umbilical cord will get compressed during delivery and not supply enough blood and oxygen to the baby.
Transverse Lie
This is a very rare position where the baby lies horizontally in the uterus. Most babies shift to a head-down position before birth. If yours doesn’t, your doctor will perform a C-section. That’s safest since there’s a small risk of what’s called umbilical cord prolapse. It’s a medical emergency in which the cord emerges before the baby.
How to Tell If a Baby Is Transverse?
As an expectant mother, it is sometimes difficult to determine what position your baby is lying in. Fortunately, there are several practical tips to help you identify what position your baby is in, particularly if it is in a transverse lie. It becomes more important to identify the baby’s position as it becomes closer to the time of delivery.
A transverse position is when the baby is lying across the womb, horizontally. Some common signs or practical tips for determining a transverse position are feeling kicks on both sides of the abdomen or having difficulty identifying a head-down position.
What Is Fetal Attitude?
Fetal attitude refers to the position of specific body parts on the baby. Examples include a baby’s chin being tucked into its chest or its legs and arms being drawn into the center of its chest. Sometimes the fetal attitude can be in an irregular position, such as the baby’s head being tilted back instead of being tucked into its chest. During the labor process, the ideal fetal attitude is when the baby’s chin is tucked into its chest and the arms and legs are drawn into its body. This allows for a much smoother labor and delivery process.
What Is Fetal Lie?
A fetal lie describes how the baby’s spine lines up with the mother’s spine. The ideal position for a fetal lie is vertical because it means the baby’s head is down in the birth canal. This is known as a longitudinal lie. If the baby is lying horizontally across the womb, it is known as a transverse lie. An oblique lie is when the baby’s head and feet rest on the mother’s pelvis. This position often means the baby will present with a shoulder or arm.
When Should a Baby Be Head Down?
Most babies assume the position they’ll be in for delivery at around 36 weeks. Before that, they may switch orientations occasionally or frequently. If your baby isn’t in the occiput anterior as labor starts, it’s safest for them if you give birth at the hospital.How to Tell if Your Baby Is Head Down
Your doctor can explain what to expect in your baby’s position in the womb from week to week and tell you specifically if your baby is head down during your appointments. You can also do what’s called belly mapping.
Using a non-toxic, washable marker, you draw on your belly to indicate where your baby’s head, buttocks, and legs are. It’s helpful to do this right after an ultrasound when the technician can show you where your baby’s heartbeat is occurring. You can then feel around for your baby’s head and buttocks and note where you sense them kicking to zero in on their legs. Many mothers enjoy the “detective work” of belly mapping.
How to Tell Baby’s Position by Kicks?
There are a few practical tips on how a mother can identify their baby’s position based on the location of the baby’s kicks. One way to identify your baby’s position based on the location of the baby’s kicks is to use a technique called belly mapping.
Belly Mapping
You can either draw on a piece of paper or with a non-toxic marker on your belly. Start by choosing a time of day when the baby is most active and when you can lie down for about 15 minutes. Tilt your belly to one side and do some deep breathing to relax. Apply gentle pressure to locate the baby’s head and bottom and mark those on your map. Next, determine if your baby is positioned spine to spine or back to belly and mark it on your map. Finally, record any movement with dotted lines on your map.
Additionally, if your belly bump feels squishy, it usually indicates that your baby is in the posterior position, or back-to-back. You may feel kicks in the middle of the belly or see some indentations around the belly button. If the baby is in the anterior position, you may feel kicks under your ribs and your belly button may look like it’s protruding.
How to Help Your Baby Assume the Best Birth Position
There are actions you can take to make it easier for your baby to get into the best position for delivery, including:
- Sit on a birth ball or exercise ball at times throughout your day.
- If you sit a lot at work, take regular breaks to stand, stretch, and walk.
- Tilt your pelvis forward (rather than backward) when sitting.
- Get on the floor on your hands and knees for a few minutes at a time a couple of times daily.
- Use a cushion on your car seat to lift your buttocks and keep your pelvis tilted forward.
- Keep your hips higher than your knees when sitting.
As for the best sleeping position to keep your baby’s head down, doctors recommend lying on your left side with a pillow between your legs.
Get World-Class Mother and Baby Care from Baptist Health
While it’s essential to understand how your baby’s position in the womb affects the birth process, it isn’t something you should worry about. Babies frequently turn just before delivery, and if they don’t, your doctor can take action to address the situation.
Learn about Baptist Health’s mother and baby care services today.
FAQ
Can a baby change from cephalic to breech?
Yes. A baby can change from cephalic to breech. Babies often shift and move positions throughout pregnancy. It is possible that a baby in a cephalic position, or head-down position, can shift to a breech position before delivery.
Will a breech baby change its position to normal?
In most cases, babies will move to a head-down or cephalic position by the 36th week of pregnancy.
How late can a breech baby turn?
Usually, if your baby has not shifted to the head-down position by week 37, your doctor may recommend different options (from a vaginal birth) for delivery. By 37 weeks, your baby has limited space to move on its own.
How should I sleep to help my breech baby turn?
Some doctors recommend sleeping on your left side with a pillow between your legs to help your baby move out of the breech position. Additionally, you can try to position your upper leg and abdomen in a forward position, allowing more of your belly to touch the bed.



